Following a typical case of mild Covid-19, SARSCoV2–specific CD8+ Tcells not only persist but continuously differentiate in a coordinated fashion well into convalescence into a state characteristic of long-lived, self-renewing memory.
— Read on www.jimmunol.org/content/207/5/1344
Tag: t-cell
Protracted yet coordinated differentiation of long-lived SARS-CoV-2-specific CD8+ T cells during COVID-19 convalescence | bioRxiv
New pre-print: “Following a typical case of mild Covid, SARSCoV2-specific CD8+ Tcells not only persist but continuously differentiate in a coordinated fashion well into convalescence, into a state characteristic of long-lived, self-renewing memory.”
— Read on www.biorxiv.org/content/10.1101/2021.04.28.441880v1
COVID-19 immune signatures reveal stable antiviral T cell function despite declining humoral responses: Immunity
COVID-19 immune signatures reveal stable antiviral T cell function despite declining humoral responses: Immunity
— Read on www.cell.com/immunity/fulltext/S1074-7613(21)00031-5
Selective and cross-reactive SARS-CoV-2 T cell epitopes in unexposed humans
Preexisting immune response to SARS-CoV-2
https://science.sciencemag.org/content/370/6512/89.full
Robust T cell responses to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus occur in most individuals with coronavirus disease 2019 (COVID-19). Several studies have reported that some people who have not been exposed to SARS-CoV-2 have preexisting reactivity to SARS-CoV-2 sequences. The immunological mechanisms underlying this preexisting reactivity are not clear, but previous exposure to widely circulating common cold coronaviruses might be involved. Mateus et al. found that the preexisting reactivity against SARS-CoV-2 comes from memory T cells and that cross-reactive T cells can specifically recognize a SARS-CoV-2 epitope as well as the homologous epitope from a common cold coronavirus. These findings underline the importance of determining the impacts of preexisting immune memory in COVID-19 disease severity.
Covid-19: Do many people have pre-existing immunity?
I have already talked about the mounting evidence supporting widespread T-cell immunity against SARS-CoV-2 (Covid-19).
This study on the British Medical Journal (Covid-19: Do many people have pre-existing immunity?) is interesting because it’s one of the few places where a similar situation from 2009 is recalled. In fact, in 2009 we experienced a casedemic with H1N1, that is, a growing number of cases which however did not lead to an actual high mortality rate. I quote:
Swine flu déjà vu
In late 2009, months after the World Health Organization declared the H1N1 “swine flu” virus to be a global pandemic, Alessandro Sette was part of a team working to explain why the so called “novel” virus did not seem to be causing more severe infections than seasonal flu.12
Their answer was pre-existing immunological responses in the adult population: B cells and, in particular, T cells, which “are known to blunt disease severity.”12 Other studies came to the same conclusion: people with pre-existing reactive T cells had less severe H1N1 disease.1314 In addition, a study carried out during the 2009 outbreak by the US Centers for Disease Control and Prevention reported that 33% of people over 60 years old had cross reactive antibodies to the 2009 H1N1 virus, leading the CDC to conclude that “some degree of pre-existing immunity” to the new H1N1 strains existed, especially among adults over age 60.15
The data forced a change in views at WHO and CDC, from an assumption before 2009 that most people “will have no immunity to the pandemic virus”16 to one that acknowledged that “the vulnerability of a population to a pandemic virus is related in part to the level of pre-existing immunity to the virus.”17 But by 2020 it seems that lesson had been forgotten.
Structural stability of SARS-CoV-2 3CLpro and identification of quercetin as an inhibitor by experimental screening – ScienceDirect
Structural stability of SARS-CoV-2 3CLpro and identification of quercetin as an inhibitor by experimental screening – ScienceDirect
— Read on www.sciencedirect.com/science/article/pii/S0141813020339970
This is on top of Quercetin also being a Zinc ionophore, which helps increasing the amount of intracellular elemental zinc, which in turns inhibits replication of RNA viruses.
Trajectory of COVID-19 epidemic in Europe and herd immunity
From this study (not yet peer-reviewed), we read:
«Whatever value is specified for the infection fatality ratio, a model that allows for heterogeneity has better fit to the data than the homogeneity model and supports herd immunity as the main factor underlying the reversal of the epidemic.»
This is compatible with the mounting evidence of pre-existing T-cell immunity against SARS-CoV-2.
Immune cells for common cold may recognize SARS-CoV-2
More on cross-reactive T-cell immunity.
They found that of the SARS-CoV-2 and “common cold” coronavirus fragments that were most similar (at least 67% genetic similarity) 57% showed cross-reactivity by memory T cells.
The evidence for pre-existing T-cell immunity against Covid-19 keeps piling up, hence the case for a much lower threshold for herd immunity becomes stronger. Conversely, the case for a vaccine becomes way weaker.
Pre-existing T-cell responses in 81% of individuals unexposed to SARS-CoV-2 (Covid-19)
This is the second study published in Nature that demonstrates cross-reactive T-cell immunity. I mentioned the other one here.
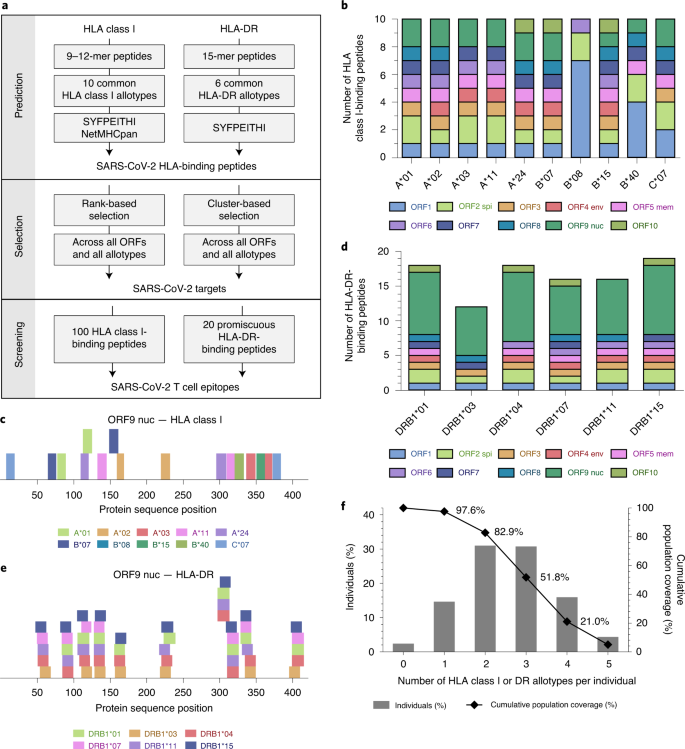
This one (SARS-CoV-2-derived peptides define heterologous and COVID-19-induced T cell recognition) says:
Cross-reactive SARS-CoV-2 peptides revealed pre-existing T cell responses in 81% of unexposed individuals and validated similarity with common cold coronaviruses, providing a functional basis for heterologous immunity in SARS-CoV-2 infection.
SARS-CoV-2-specific T cell immunity in people that never had Covid-19
For all those who like to dismiss papers when they are either not yet peer-reviewed or published on journals that are not exactly mainstream, here is a paper published in Nature:
SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls
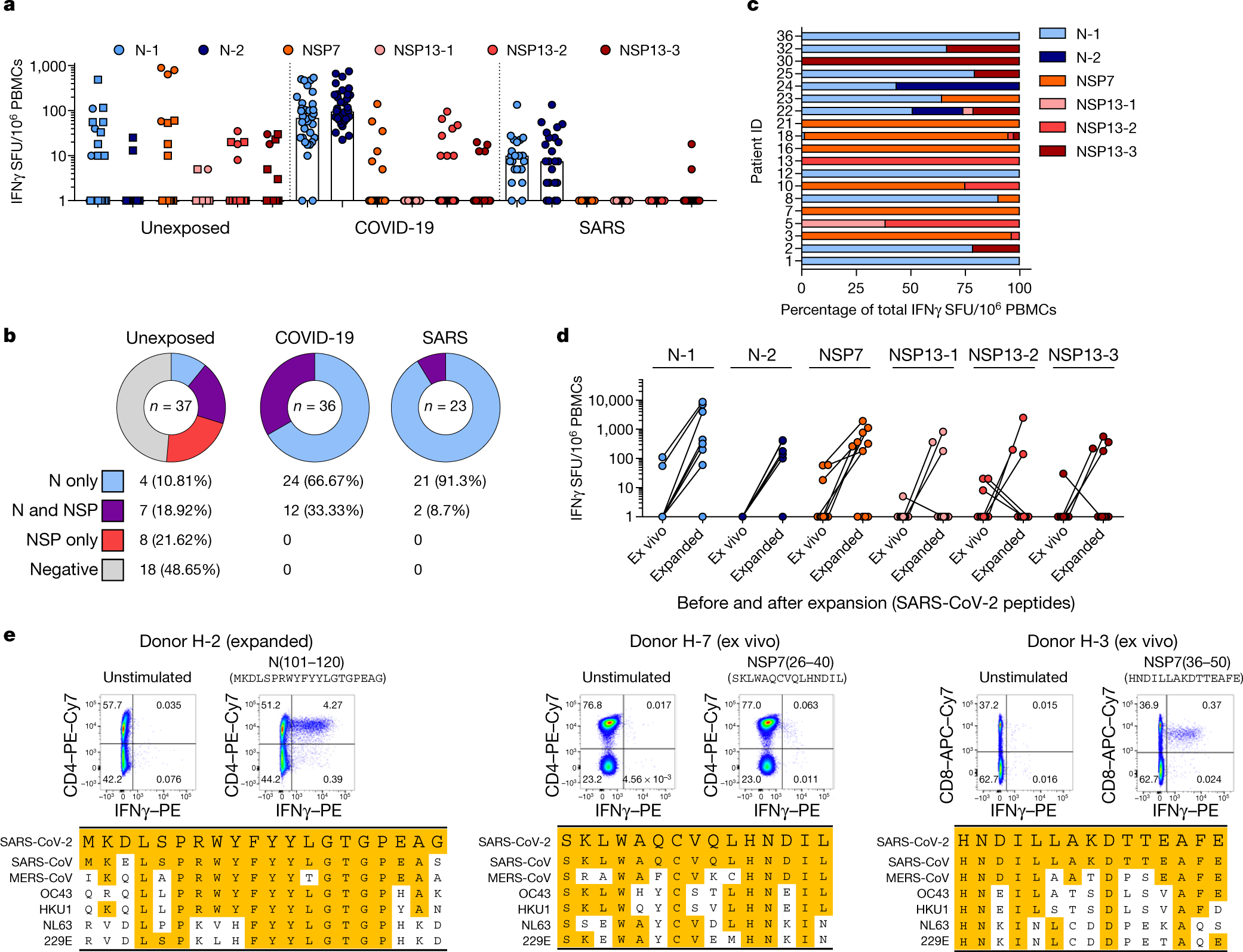
In short:
- Covid-19 infection obviously creates T-cell immunity which long lasting and will protect people who recovered from ever getting Covid-19 again
- People who caught SARS-CoV-1 (the first SARS) also have long lasting T-cell immunity (still working 17 years later) that works against Covid-19 (SARS-CoV-2)
- Roughly 50% of the tested subjects who never caught either SARS viruses also had T-cell immunity that worked against Covid-19 due to a high degree of homology to the sequences of some proteins common to both SARS-CoV-2 and the common cold coronaviruses.