Following a typical case of mild Covid-19, SARSCoV2–specific CD8+ Tcells not only persist but continuously differentiate in a coordinated fashion well into convalescence into a state characteristic of long-lived, self-renewing memory.
— Read on www.jimmunol.org/content/207/5/1344
Search: “t-cell”
We found 25 results for your search.
Longitudinal analysis shows durable and broad immune memory after SARS-CoV-2 infection with persisting antibody responses and memory B and T cells: Cell Reports Medicine
Longitudinal analysis shows durable and broad immune memory after SARS-CoV-2 infection with persisting antibody responses and memory B and T cells: Cell Reports Medicine
— Read on www.cell.com/cell-reports-medicine/fulltext/S2666-3791(21)00203-2
Yet another study confirming both B and T cell long lasting and stable immunity in Covid-19 recovered patients. Those who have had Covid-19 DO NOT NEED the vaccine. Yet in many countries they are being threatened with #GreenPass, which can only be kept “Green” with regular doses of vaccine.
Immunodominant T-cell epitopes from the SARS-CoV-2 spike antigen reveal robust pre-existing T-cell immunity in unexposed individuals | Scientific Reports
The COVID-19 pandemic has revealed a range of disease phenotypes in infected patients with asymptomatic, mild, or severe clinical outcomes, but the mechanisms that determine such variable outcomes remain unresolved. In this study, we identified immunodominant CD8 T-cell epitopes in the spike antigen using a novel TCR-binding algorithm. The predicted epitopes induced robust T-cell activation in unexposed donors demonstrating pre-existing CD4 and CD8 T-cell immunity to SARS-CoV-2 antigen. The T-cell reactivity to the predicted epitopes was higher than the Spike-S1 and S2 peptide pools in the unexposed donors. A key finding of our study is that pre-existing T-cell immunity to SARS-CoV-2 is contributed by TCRs that recognize common viral antigens such as Influenza and CMV, even though the viral epitopes lack sequence identity to the SARS-CoV-2 epitopes. This finding is in contrast to multiple published studies in which pre-existing T-cell immunity is suggested to arise from shared epitopes between SARS-CoV-2 and other common cold-causing coronaviruses. However, our findings suggest that SARS-CoV-2 reactive T-cells are likely to be present in many individuals because of prior exposure to flu and CMV viruses.
— Read on www.nature.com/articles/s41598-021-92521-4
Protracted yet coordinated differentiation of long-lived SARS-CoV-2-specific CD8+ T cells during COVID-19 convalescence | bioRxiv
New pre-print: “Following a typical case of mild Covid, SARSCoV2-specific CD8+ Tcells not only persist but continuously differentiate in a coordinated fashion well into convalescence, into a state characteristic of long-lived, self-renewing memory.”
— Read on www.biorxiv.org/content/10.1101/2021.04.28.441880v1
Exposure to SARS-CoV-2 generates T-cell memory in the absence of a detectable viral infection | Nature Communications
Basically, as I had predicted from a Japanese study from months back, asymptomatic people spread immunity. Immunity! And lockdowns have slowed that down!
— Read on www.nature.com/articles/s41467-021-22036-z
COVID-19 immune signatures reveal stable antiviral T cell function despite declining humoral responses: Immunity
COVID-19 immune signatures reveal stable antiviral T cell function despite declining humoral responses: Immunity
— Read on www.cell.com/immunity/fulltext/S1074-7613(21)00031-5
Immunodominant T-cell epitopes from the SARS-CoV-2 spike antigen reveal robust pre-existing T-cell immunity in unexposed individuals | bioRxiv
Selective and cross-reactive SARS-CoV-2 T cell epitopes in unexposed humans
Preexisting immune response to SARS-CoV-2
https://science.sciencemag.org/content/370/6512/89.full
Robust T cell responses to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus occur in most individuals with coronavirus disease 2019 (COVID-19). Several studies have reported that some people who have not been exposed to SARS-CoV-2 have preexisting reactivity to SARS-CoV-2 sequences. The immunological mechanisms underlying this preexisting reactivity are not clear, but previous exposure to widely circulating common cold coronaviruses might be involved. Mateus et al. found that the preexisting reactivity against SARS-CoV-2 comes from memory T cells and that cross-reactive T cells can specifically recognize a SARS-CoV-2 epitope as well as the homologous epitope from a common cold coronavirus. These findings underline the importance of determining the impacts of preexisting immune memory in COVID-19 disease severity.
Pre-existing T-cell responses in 81% of individuals unexposed to SARS-CoV-2 (Covid-19)
This is the second study published in Nature that demonstrates cross-reactive T-cell immunity. I mentioned the other one here.
This one (SARS-CoV-2-derived peptides define heterologous and COVID-19-induced T cell recognition) says:
Cross-reactive SARS-CoV-2 peptides revealed pre-existing T cell responses in 81% of unexposed individuals and validated similarity with common cold coronaviruses, providing a functional basis for heterologous immunity in SARS-CoV-2 infection.
SARS-CoV-2-specific T cell immunity in people that never had Covid-19
For all those who like to dismiss papers when they are either not yet peer-reviewed or published on journals that are not exactly mainstream, here is a paper published in Nature:
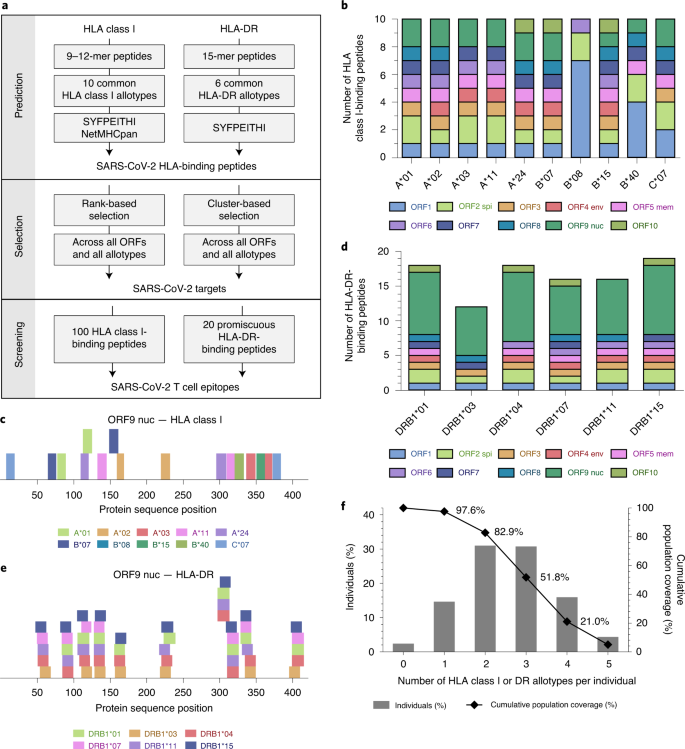
SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls
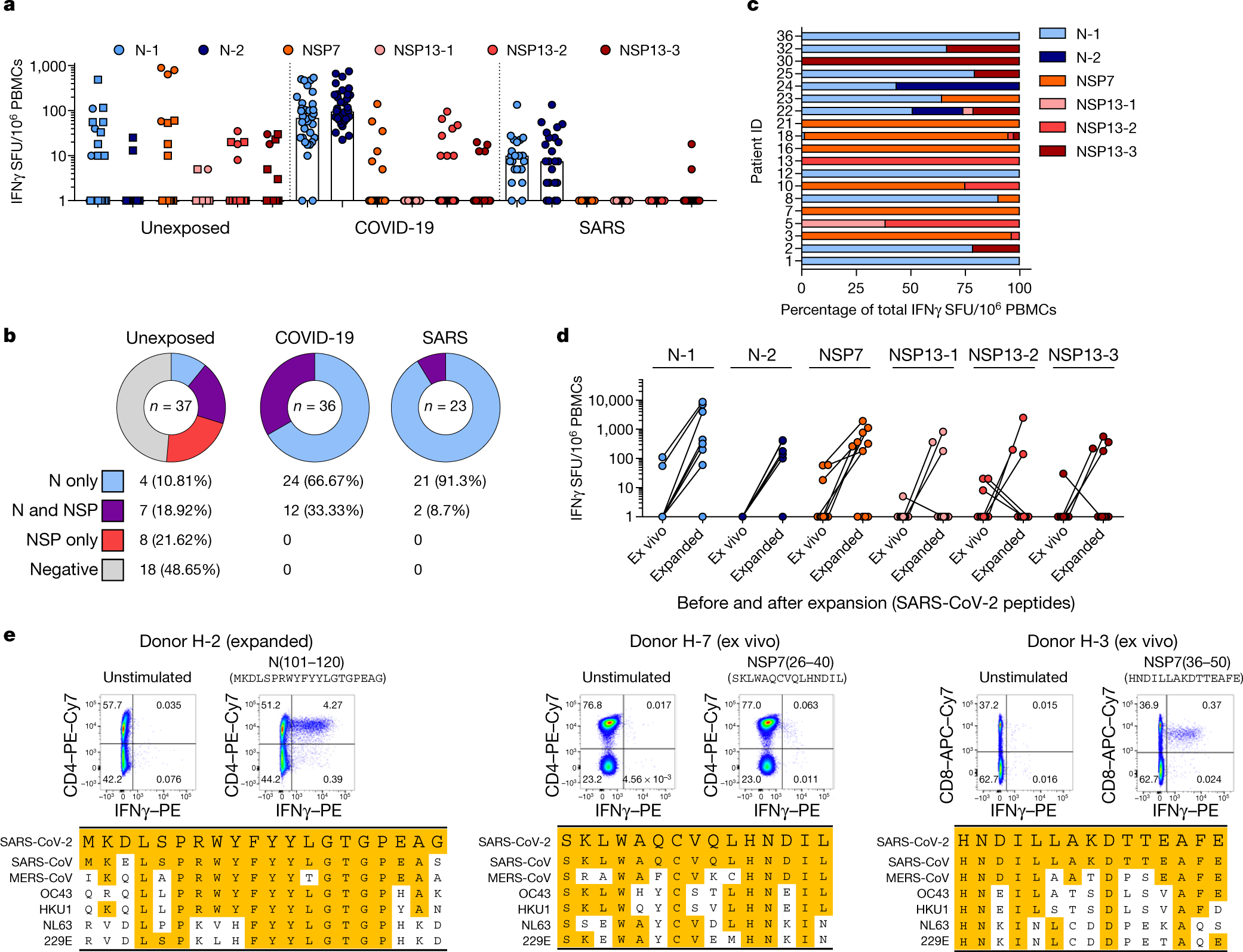
In short:
- Covid-19 infection obviously creates T-cell immunity which long lasting and will protect people who recovered from ever getting Covid-19 again
- People who caught SARS-CoV-1 (the first SARS) also have long lasting T-cell immunity (still working 17 years later) that works against Covid-19 (SARS-CoV-2)
- Roughly 50% of the tested subjects who never caught either SARS viruses also had T-cell immunity that worked against Covid-19 due to a high degree of homology to the sequences of some proteins common to both SARS-CoV-2 and the common cold coronaviruses.